Amniotic Fluid Embolism (AFE) is a rare yet catastrophic complication that can occur during labor or immediately after childbirth. It poses a significant risk to both mother and baby and remains one of the leading causes of maternal mortality in the USA.
Understanding the causes, risk factors, symptoms, and treatment options for AFE is crucial in managing and preventing this life-threatening condition. Despite the rarity of the occurrence, heightened awareness among healthcare professionals and pregnant individuals is key to ensuring rapid intervention, which can improve survival rates and long-term outcomes for both the mother and baby.
Causes and Risk Factors
What Causes Amniotic Fluid Embolism?
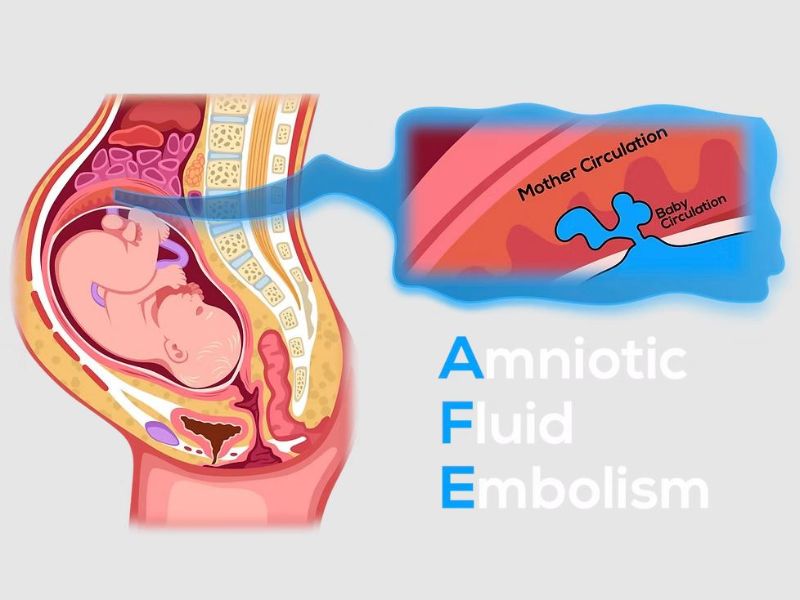
The exact cause of amniotic fluid embolism is still not fully understood. However, it is believed to occur when amniotic fluid, fetal cells, or placental material enters the maternal circulation, triggering a catastrophic immune response. The amniotic fluid can pass into the bloodstream through the cervix, uterus, or placental site during labor or delivery. When this foreign material enters the bloodstream, it can cause severe reactions, including allergic responses, blood clotting disorders, and cardiovascular collapse.
AFE often happens suddenly and without warning, leading to immediate medical emergencies. The mechanisms behind this embolism are not completely understood, but it is theorized that the amniotic fluid contains substances that cause a systemic inflammatory response when introduced into the maternal system.
Risk Factors for AFE
While the exact causes are still being researched, certain risk factors have been identified that may increase the likelihood of developing AFE. These include:
- Advanced Maternal Age: Women over the age of 35 are more likely to experience pregnancy complications, including AFE.
- Multiple Pregnancy: Women carrying twins or other multiples are at an increased risk due to the larger amount of amniotic fluid and the increased likelihood of complications.
- Placental Complications: Conditions such as placenta previa (where the placenta covers the cervix) and placental abruption (where the placenta separates from the uterine wall prematurely) have been linked to AFE.
- Cesarean Section or Instrumental Deliveries: Surgical deliveries, especially emergency C-sections, may involve procedures that increase the likelihood of the amniotic fluid entering the maternal bloodstream.
- Induced Labor: Use of induction medications such as oxytocin or prostaglandins has been noted as a potential trigger for AFE.
- Preeclampsia/Eclampsia: Women with hypertensive disorders during pregnancy are at higher risk.
Though rare, women with one or more of these risk factors may be more susceptible to experiencing AFE, though it can still happen unpredictably.
Symptoms and Clinical Presentation
The symptoms of amniotic fluid embolism usually develop suddenly and can escalate quickly. The most common symptoms of AFE include:
- Respiratory Distress: One of the hallmark symptoms of AFE is a sudden onset of shortness of breath. The woman may feel as though she cannot catch her breath, often progressing to complete respiratory failure if not treated immediately.
- Cardiovascular Collapse: AFE often leads to a sudden drop in blood pressure (hypotension), arrhythmias, and in severe cases, cardiac arrest.
- Disseminated Intravascular Coagulation (DIC): This is a blood clotting disorder that causes uncontrollable bleeding throughout the body. DIC is a common and serious complication associated with AFE.
- Neurological Symptoms: Seizures, confusion, loss of consciousness, or altered mental status can occur due to the disruption in oxygen supply to the brain.
- Fetal Distress: In cases of AFE occurring during labor, fetal distress may be noted, often manifested as a significant drop in the fetal heart rate, which may signal the need for immediate emergency intervention.
These symptoms can be severe and rapid in onset, which makes AFE particularly dangerous. The speed at which the condition progresses makes it crucial for healthcare providers to diagnose and treat the complication as quickly as possible.
Diagnosis
Diagnosing AFE can be difficult because the symptoms overlap with other conditions that may occur during or after childbirth, such as pulmonary embolism, anaphylactic reactions, or eclampsia. The diagnosis is largely clinical, with healthcare providers relying on a set of criteria that includes the sudden onset of cardiovascular and respiratory collapse, along with laboratory signs of DIC. Diagnostic procedures may include:
- Clinical History: Reviewing the patient’s labor and delivery details, including the presence of risk factors and the sudden onset of symptoms.
- Blood Tests: Indicators of DIC, such as low platelets, elevated clotting times, and fibrinogen depletion, can help support the diagnosis.
- Exclusion of Other Conditions: AFE must be differentiated from conditions such as pulmonary embolism, anaphylaxis, and sepsis, all of which have similar presentations.
In the U.S., hospitals with high-risk obstetric care units are better equipped to diagnose AFE using advanced monitoring tools, but diagnosis remains challenging.
Treatment and Management
Since AFE is a medical emergency, immediate treatment is critical for the survival of both mother and child. Treatment primarily focuses on supportive care and addressing the underlying symptoms.
Initial Management
- Oxygen Therapy: The first step is to administer oxygen to help manage the respiratory distress. Many patients will require mechanical ventilation to maintain adequate oxygen levels.
- Cardiovascular Support: Blood pressure will need to be stabilized through intravenous fluids, vasopressors, and medications to restore circulation.
- Blood Transfusions: Because of the blood clotting abnormalities (DIC) that occur with AFE, blood transfusions and clotting factor replacement are often necessary to address bleeding complications.
- Seizure Control: If seizures occur, they must be controlled with appropriate anti-seizure medications.
- Emergency Delivery: In cases of AFE occurring before or during labor, an emergency cesarean section may be required if fetal distress is present.
The rapid administration of these interventions is essential, and in most cases, the mother will be transferred to an intensive care unit (ICU) for continuous monitoring.
Prognosis and Outcomes
Despite improvements in medical care, AFE is still associated with high mortality rates. Maternal survival rates vary, but studies suggest that 20-60% of women who develop AFE survive the condition, with some survivors facing long-term neurological impairment due to oxygen deprivation during the event.
Impact on Newborns
Neonatal outcomes depend on the timing of the event and how quickly medical teams can respond. Babies born during an AFE episode are at risk of hypoxia and can suffer from brain injuries or developmental delays. Immediate neonatal care is essential to mitigate potential complications.
Prevention and Future Research
There are currently no known ways to definitively prevent AFE, as it occurs unpredictably. However, continued research is being conducted to:
- Identify Early Risk Indicators: Some studies are exploring biomarkers that may signal an increased risk for AFE, which could allow for early intervention.
- Improved Emergency Protocols: Hospitals are continually refining their protocols to improve response times and outcomes in AFE cases.
- Advancements in Critical Care: Further development in critical care medicine, including ECMO (extracorporeal membrane oxygenation), is offering hope for improved survival rates.
Amniotic Fluid Embolism is a rare, but potentially fatal, complication of childbirth that requires rapid diagnosis and intervention. Although the exact cause remains elusive, healthcare professionals are becoming better equipped to manage this emergency, improving survival rates for both mothers and babies. Awareness of risk factors and symptoms, along with the continued advancement in maternal healthcare, will play a significant role in reducing the impact of AFE in the future. With more research, better preventive measures, and quicker response times, it is possible to improve the outcomes for women facing this life-threatening complication in the USA.